“A child born to another woman calls me mommy. The magnitude of that tragedy and the depth of that privilege are not lost on me.”
Have you seen that meme? It captures my feelings towards birthmothers in general, and Patrick’s birthparents in particularly so perfectly. I feel it to the core of my being.
It also only captures a fraction of the unrepayable debt of gratitude that I owe as a mother.
Another child was lost young in an accident, and that family chose in the face of unimaginable loss to give a piece of the life of their child to mine through organ donation. That is tragedy so vast and privilege so profound I struggle to comprehend it.
The pandemic has pushed this truth to the forefront of our awareness. “Patrick’s a transplant recipient” is a phrase we say so often it sometimes loses meaning. It tells you he has health problems that require extra accommodations. It may even tell you his health is fragile or that he’s been through a lot of trauma.
But in our house, lately, we’ve had a lot of discussion about what transplant actually IS. See, Patrick received his transplant the day he turned 6. He was too young and had far too little language and understanding to know what was happening to him then. But there’s nothing like a pandemic to provide time for questions and answers.
Patrick has some fairly distinct memories of his recovery. The staples itched. The stitches were blue. But many of the memories are fading. (“Mom, what’s an ostomy?”) He’s twelve and a half, more than double his age at transplant. Early childhood memories fade and our minds protect us from trauma. He remembers feelings, but very few details.
This week, he found a memento of transplant: a pillow in the shape of a liver with the hospital logo emblazoned on it that was signed by many of the ICU staff. Patrick loved writing and names, so it was a way he connected and found peace.

I can’t put faces to most of the names anymore. But as we talked, I pointed out how many of them had written their specialty and that could tell us who they were. Nurses helped with pain and meds and dressings and keeping him comfortable. Respiratory therapy would come to make him take deep breaths and refill his lungs, since it hurt too much to breathe, let alone willingly cough. And child life made sure he had toys and volunteer visitors fun activities and the occasional magic moment.


One of the signatures was from the physical therapist. She’s one of the only faces I clearly remember. I told him how she came every day to help him learn to walk again and how, at first, that was very hard because it was so painful. (I also told him about how much he loved her because she would hide Blues Clues in the halls for him to find.)
That led to talking about his scars.
Patrick had a vertical incision that ran the length of his abdomen that was closed with staples and, as a result, he has a very impressive scar. We talked about what he remembered about how that looked and felt. Then he turned his attention to other scars. He has all kinds: from big to small, from straight to round and some that are curvy. Some are surgical, some from his birth defect, and others from accidental injuries. And he made me help him inspect his entire body and tell him how each one got there. Sadly, there really is a scar and a story for almost every appendage.

“Why” has been a big topic of conversation lately. We’ve had to answer a lot of “Why’s” about the COVID precautions we are taking. And a lot of why’s about other people who are not longer taking them. And in the middle of one of those “why” we still wear masks when others don’t, it occurred to me that Patrick knew “transplant” as part of his identity, but didn’t understand what the word meant.
I’ve been thinking that, since we moved and so much time has passed, many of our friends, colleagues, classmates and fellow congregants don’t know the why and how either. So, since we’re already opening the emotional pandora’s box by explaining these things to Patrick, I thought maybe I’d tell you what I’ve been telling him.
Let me take you on a tour of his scars.
(Just a heads up, Patrick is very private about his scars and doesn’t like to talk about what he’s been through.)
First, there’s the short little horizontal one that runs to the right of his belly button. This one’s from his gastroschisis. Gastroschisis is a birth defect where the abdominal wall doesn’t close and the intestines develop outside of the body. This was the start of his troubles. Patrick had complicated gastroschisis. The intestines twisted and died. He was born with a small hole in his belly. The surgeons did a quick exploratory surgery where they found that his entire small intestine and most of his large intestine were missing. They placed some drain tubes (since his intestine was too short and too narrow to reconnect) and closed the hole surgically. They also placed a PICC (peripherally inserted central venous catheter) to give him nutrition by IV as his digestive system was completely non-functional.
A few weeks later, those drains weren’t working. So they pulled the end of his duodenum to the skin’s surface in an ostomy (which means a hole in your body that accesses an organ) and placed a feeding tube in his belly. (That tube is still there, used for meds, not food.)

We were granted guardianship and flew him from Michigan to Utah by air ambulance. A short time later, he developed his first central line infection while still in the NICU. He has a scar on the back of his right heel where a busy nurse missed that the IV antibiotic being given there had caused the vein to burst. This caused a nasty IV infiltration wound. He also earned his first broviac line scar. (Broviac lines are also central lines, they run to the heart.. but they go in a tunnel through the chest. Patrick’s chest and neck have several pock-mark looking scars from broviac lines.)
The next 5 years were spent waiting for transplant. Beginning in July of his first year and continuing for the next year, he seemed to have constant sepsis. We’d clear one infection, and two weeks later be back in the E.R. with another. It was terrifying, especially when yeast started to grow inside his body. Yeast is sticky and difficult to kill. The antifungals used to treat it are harsh. Eventually, their toll was too much for his little body and his heart stopped.
This left scars you can’t see in the form of an anoxic brain injury, but also a new little one in his thigh from a femoral arterial line. It also left some emotional scars for all of us. We were fortunate that, because the amazing team at the hospital that day performed such excellent CPR, he was revived and has such minor damage. Still I know what it is to have my child stop breathing in my arms. And I know what it is to have arms ache for a baby that isn’t there. We live with the effects of that day constantly.

At 9 months old, Patrick’s first transplant team said they didn’t want him to have an ostomy anymore. So a surgeon here in Utah connected his duodenum (the segment between stomach and small intestine) to his large intestine. That incision was a small vertical one next to his belly button. It left his belly looking like a star and we lovingly called him our star-bellied sneech.

Over the next 5 years, he had lots of lines, another surgery, a couple of liver biopsies, and significant scarring inside his major blood vessels from his chronic need for total parenteral nutrition and the accompany central lines. His veins became so scarred that we though he might lose access to IV nutrition and starve, but the interventional radiology team in Nebraska managed to restore access through a very risky procedure than passed a needle tipped catheter up his femoral vein, through his heart and out his jugular.
He had IV pumps in a backpack that he took with him everywhere he went that provided him with nutrition in the form of TPN and lipids. Not having an intestine meant a chronic diarrhea and vomiting, too, so we had one more pump for IV hydration fluids, and the occasional extra pump running broad spectrum IV antibiotics. We carried a diaper bag full of saline and heparin syringes and emergency kits, along with an epi pen (he had several serious food allergies) everywhere we went. We were pros at swapping out broken IV tubing, performing sterile dressing changes, and clearing air in line issues in the dark without waking the child the tubing was attached to. I knew every creaky spot in the floor and could dance through the room without a sound, kind of like a master criminal weaving through security system lasers.

We kept our GI and the emergency room on speed dial. We knew every member of the resident class at Primary Children’s spanning several years. (They made a point to come visit us when they knew we were there.) And I spent more time talking to our infusion pharmacist and insurance case manager than most of my friends.
Meanwhile, Patrick grew up, went on many adventures, attended preschool, started kindergarten, and was granted a wish.

At last, Patrick received his transplant. He not only needed an intestine, but also a liver due to damage from the IV nutrition, and since the vasculature is all one package, that came with a new pancreas, too. Remembering how HUGE an intestine is, it might make more sense to know that they also removed his spleen to make space along withhis gall bladder because that way they don’t have to worry about gall stones later. They also did a gastric bypass to help food move into the new anatomy of the gut.
As I explained to Patrick this week, they pretty much just took everything out so it was empty inside, and then put in the new organs and sewed all the parts back together. And that is a LOT of parts when you consider all the blood vessels, nerve endings and splicing back together his lymphatic system.

Transplant left the biggest scars: the long one down his tummy with the frankenstein-like staple marks and the one the size of a silver dollar where he had an ostomy for biopsy purposes.
That brings me back to the “why” questions. Because transplant and the journey to get there are why we do most of what we do.
So here’s a question we get a lot.Why are transplant patients more at risk that other people? Doesn’t a transplant cure them?
This answer was one they drilled into us. When you’re being considered for transplant, they sit down with your family and they go over all the risks and precautions that you’ll be living with after the procedure. You also commit to a lot of things to protect the graft like avoiding contact sports, not swimming in rivers and lakes, and being careful about diet.
And then of course, there are the meds. To keep the body from identifying the transplanted organs as a threat, transplant patients must take immune suppressants. Twice a day, every day. For the rest of your life. These have to stay at a constant level in the body.
At first, immune suppressants have to be at a pretty high dose. Eventually, as the body gets used to the new organs, that dose can be reduced. However, since Patrick received 3 organs (including the second largest organ in the human body) his minimum dose is still high compared to, for example, a kidney transplant patient.
Still, with a lower dose, Patrick has been able to live a pretty normal life. He could attend school, except when there was an outbreak of illness in the classroom. (His IEP provides for home learning under these conditions.) He could go to church and play adaptive sports and ride roller coasters. Granted, he and I spend pretty much from November to February sick every year because he catches everything he’s exposed to. Transplant patients get sicker and stay sicker longer, but eventually, he gets over most bugs.
But COVID… it’s a different type of virus. It sends the body’s immune system into hyperdrive. That’s what makes it so deadly. Can you imagine the effect of that in a transplant patient?
I wondered if perhaps it was my imagination inflating the risks at first. However, a few months back as they were just about to approve the pediatric Pfizer vaccine, I had the opportunity to join a webinar where researchers shared their current data about COVID, the COVID vaccines, and transplant patients. And some of their numbers were rather concerning.
First, they found that although the general population has a better than 99% chance of surviving the virus, among transplant patients, the death rate is 10%. Those odds are scary.
Even more concerningly, Johns Hopkins, in the absence of data from preliminary studies into vaccines, did a study where they measured the antibody response of transplant patients. As the researcher said in his presentation, they discovered that “we have a problem.” Only around 40% of transplant patients had any detectable antibodies following a first dose of any of the vaccines. After the second dose, only 56% did. They also found that there was a high rate of patients who resumed normal activities after they were “fully vaccinated” who went on to contract the virus.
You know when they say that most people who are vaccinated don’t catch the virus, don’t pass it on to others, and certainly don’t need hospitalization or die? Well, guess who that small percentage who do are? Yup, the people with compromised immune systems.
So EVERY communication I have with Patrick’s transplant team or GI doctor ends with a reminder. “Act like he’s not vaccinated.” “Keep following precautions.” “There’s still risk.” Just this week, Patrick’s GI ended an e-mail about lab results with “don’t let down your guard.”

The thing is, everyone is ready to be done with the pandemic. WE are ready to be done with the pandemic. In fact, the more our community lets down their guard, the harder it becomes for us.
But cases are rising across the world, across the country, and definitely in the state where we live. Vaccination rates are low here and children, though not at risk of severe disease, are still carriers. Add to it that the Delta (now Delta+) variant is more contagious and more deadly. Despite our best wishes, statistics show that the virus is no longer in decline where we live.

We made a commitment years ago. We made it when we adopted him, again when we listed him for transplant, and again when we accepted the offered organs. We promised that we would follow the medicine, keep the protocols, and make the sacrifices to keep him alive.
Patrick’s life is a miracle. Many times over. And that miracle has been contributed to by so many people. His birth family, the NICU teams, his nurses, and pharmacists, the surgeons and infectious disease doctors and interventional radiologists and IV team who responded to emergency after emergency. The nurse who performed CPR and the code team who helped to revive him. The therapists who taught him to walk and talk and write. The family and friends and strangers who helped raise money for his transplant expenses. And most of all, the family who trusted their memory of their child to the future of mine.
In coming to understand transplant, Patrick’s come to know that he has an organ donor. The other night, he was asking me about “the other kid.” Health privacy means we don’t know a lot. But often, when I’m tempted to take some risk, Patrick’s donor and his family cross my mind. I can’t bring myself to take chances with such a sacred gift. Especially when there are so many waiting for donors who will not live to be matched.
We live with a miracle every day. But faith without works, as James wrote, is dead. So we are doing our best to do our part and be patient until we get the all clear from the miracle workers we’ve grown to trust to keep Patrick safe. Some of them are like family, so when they say wait, we listen.
We are hopefully trusting in the promise of vaccines. I was able to enroll Patrick in that same Johns Hopkins vaccine antibody study for kids and we’re watching to see signs of his body reponding to the shot. (With caution, as every doctor emphasizes to us that antibodies do not mean he can’t get sick.)
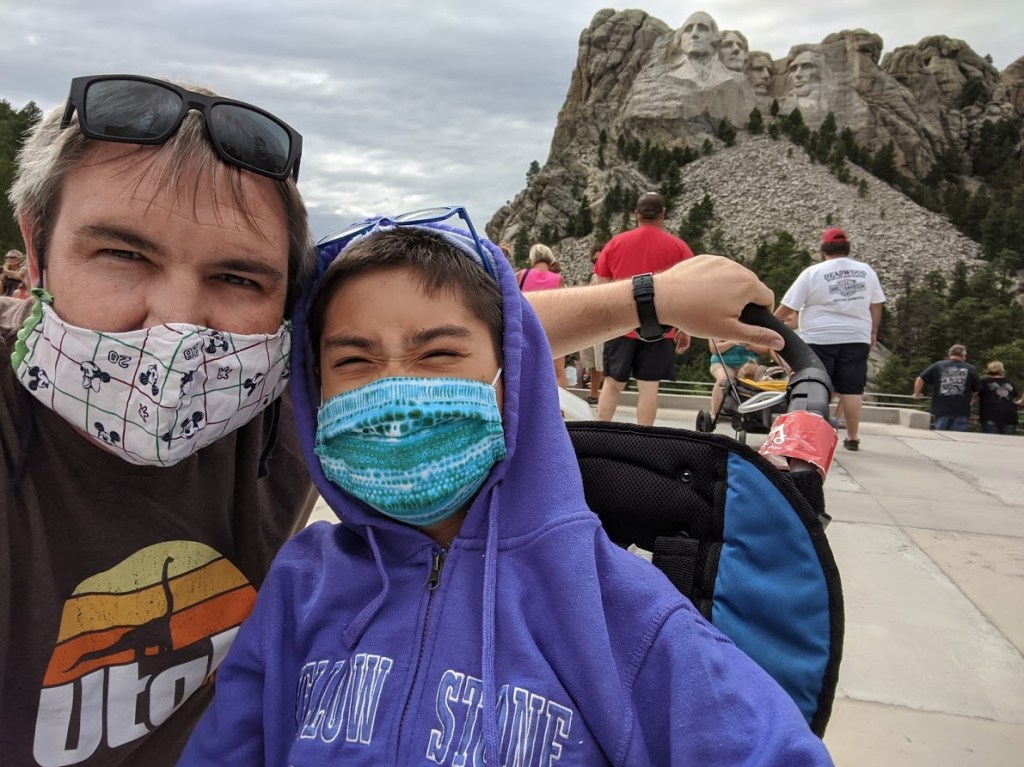
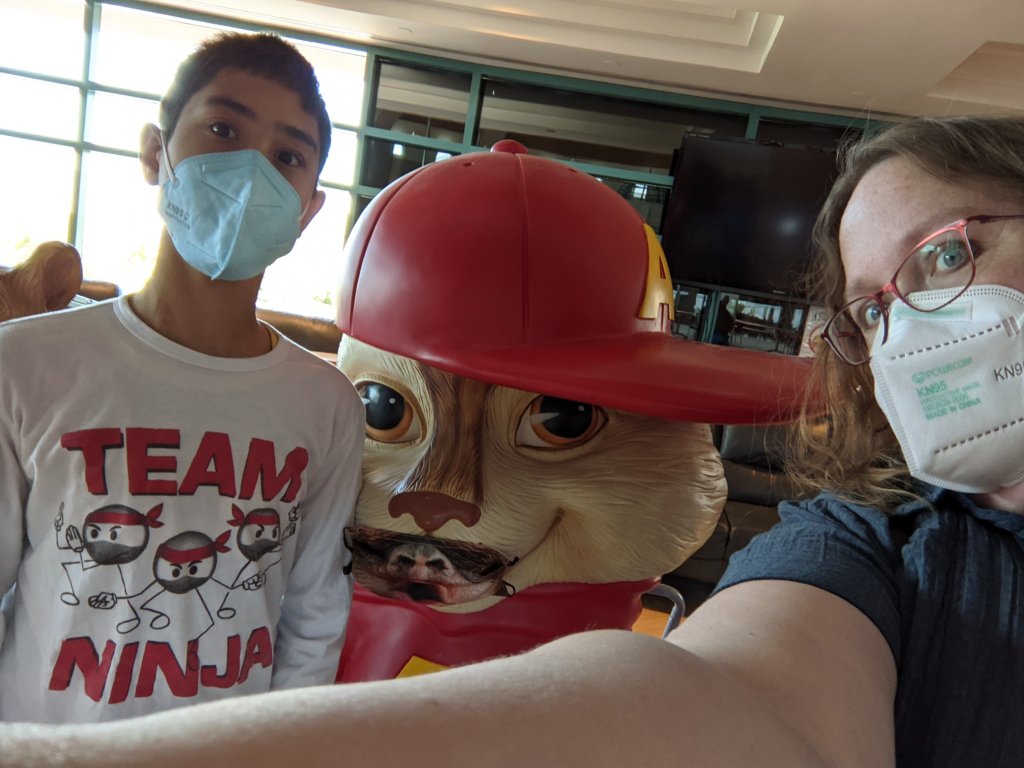
We are cautiously beginning to dip our toes in. We are visiting with fully vaccinated (and still reasonably cautious) family. I’ve invested in KN95 masks that fit Patrick and am letting him go to in-person physical therapy and occasional uncrowded places in off-peak hours, like the library.
We really want to begin to allow loved ones back into our world and are anxiously waiting for approval of vaccines for younger children.
We want to see you again. Right now, we’re limited contact to vaccinated people. So help us out. Get the shot. Wear your mask indoors and in crowds and around us. Avoid risky behaviors.
Be especially careful with your children. Not only can they spread COVID, but there’s an out of season cold and flu season happening as we come out of quarantine and their risk of catching another illness is higher right now. Please stay home if you have any signs of illness! (Even when we were really counting on you.)
This is an awkward time right now. For everyone. But especially for us. With the political climate and the need for extra caution, we sometimes have to turn down invitations or even walk away when risk is too high. If one of these awkward moments happens with you, please know that we don’t mean to cause offense. We’re not trying to make you feel guilty or sway your choices. (Though we really want you to be safe.) It’s just, with all other precautions taken away, we are needing to be a lot more careful.
We appreciate your patience, your love, your caution, your efforts to keep us included and show us we are remembered. We are eager to be with you again. And we are THRILLED that vaccination has brought some of your back into our lives in person. Patrick’s very best days are when we can say “So-and-so has had their shot. Let’s go do something together!” Hoping for much, much more of that soon.















