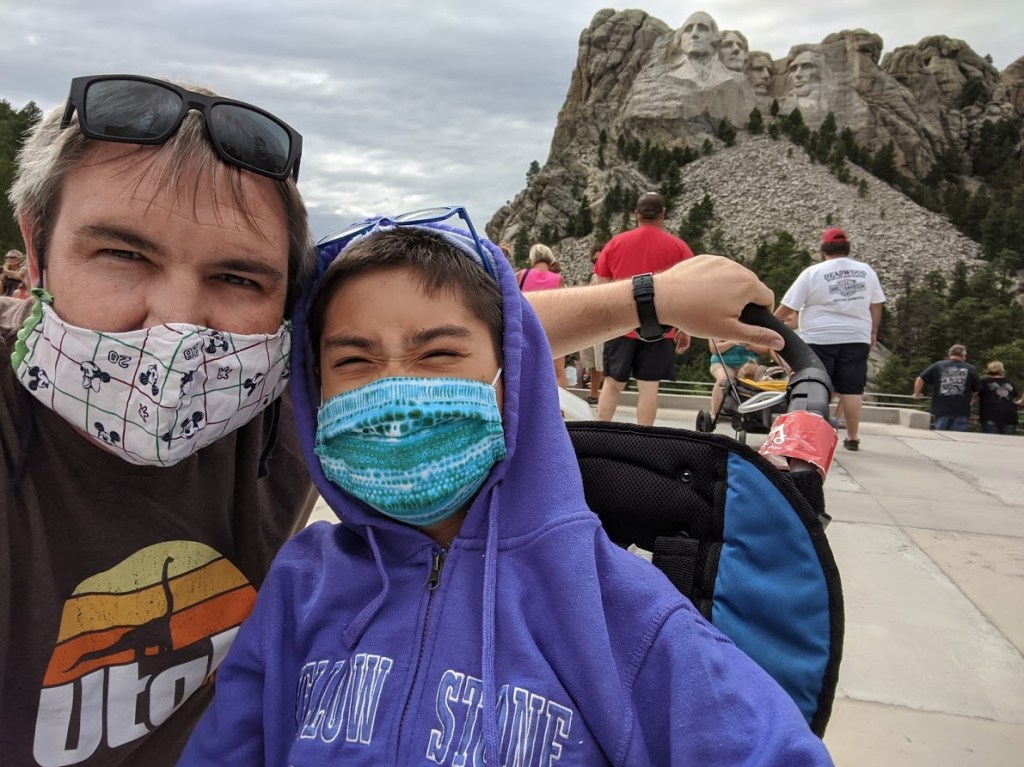
Ok. Technically, this is being written several days after day 3,653. That’s because we just got home from a week celebrating in Disneyland. That was Patrick’s pick, but there really isn’t any better place to celebrate magic, dreams, wishes.
This has been a really emotional week… month… fall?..!!
I always get nostalgic in October. This year, even more so, however. That has a lot to do with transplant. We took Patrick’s trip for his annual checkup early because we wanted to celebrate his transplant anniversary over his birthday. It just happened that we were there over the same week he’d taken his wish trip ten years before. Then, just a few weeks ago, my niece had a baby boy who spent 20 days in the NICU, so we have spent a lot of time in and out of that familiar setting again.

There have been a lot of reminders around what was already bound to be a very nostalgic anniversary.
Getting ready for our trip, I stayed up late wrapping Patrick’s birthday presents so he could open then in the morning right before we left. We’ve been so busy with work, school, family, and getting ready that I just ran out of time.
I try not to put off wrapping the presents. The night before Patrick’s transplant, I also stayed up late wrapping his presents because the week had been busy and I hadn’t gotten to it. I’d just wrapped those presents, gotten in bed, and switched out the lights when my phone rang and the caller ID lit up with the number of the transplant hospital. That number at 10 p.m. could only mean one thing… And I didn’t want to take that call on my little boy’s birthday eve.
Still, we packed the presents that could travel and we went.
I was so afraid to take that call. It was so scary to say yes, to pack our bags, to wake our little boy, and to fly all night to turn our little boy over to an uncertain fate.

One of the hardest things about intestinal transplant was that, with TPN, you aren’t actively getting sicker. You don’t see a child who is getting visibly sicker the longer they are on the transplant list. In fact, Patrick seemed so healthy. He was having one of the best years of his life. He was loving kindergarten.
Health doesn’t decline gradually with short bowel syndrome. The scary moments ambush you. Patrick would be fine, then suddenly, he’d have a fever and we’d be rushing to the hospital to be treated for sepsis. Or he’d catch his line and it would break. Or a clot would form so we couldn’t use it. We could go months in peace, but when things went wrong, we were rushing to the emergency department. Behind the scenes, he was running out of central venous access and the situation was getting worse. We knew one day, he’d run out of veins for the IVs that were feeding him, and that would happen with no warning. It was like living with a ticking time bomb. One that would alarm at random to remind us time was running down.
When he was not quite 5, Patrick ran out of major vessels above his heart where central lines could be placed. It happened suddenly. A doctor wrote the wrong concentration of ethanol lock. A line clotted. A nurse flushed too hard. Patrick went to surgery to have the line replaced and he came back without one. Upon hearing the news, the transplant team made him status 7 on the transplant list — on hold. Without access, he could not have a transplant. Two days later, we flew to Nebraska to have an alternative central line placed by passing a sheathed needle through his femoral vein and through his heart and out through his superior vena cava.

That’s when we knew that without a transplant, Patrick was unlikely to survive many more years.
A year later, just before Patrick’s 6th birthday, he was granted a wish by Make-a-Wish Utah and we took him to Disneyworld and Give Kids the World Village in Orlando. He’d been listed for a year and a half in Nebraska by then – 5.5 years total – with no match. He was on his second alternate line.
A month later, Patrick got THE call. A donor had finally been found.
That was ten years ago.

Our villa and rental car are in the background.
We just celebrated Patrick’s sixteenth birthday. I never imagined sixteen. I hadn’t really imagined a ninth birthday.
This life has made us a bit shy about looking too far into the future. On the other hand, we are very good at living in the moment and very grateful for every milestone.
Sixteen and ten years since transplant are big ones.
Most of the published data about transplant stops giving numbers after 10 years. Way back when we first listed Patrick for transplant, the procedure was still extremely new and borderline experimental. It was a little more mainstream 6 years later when we finally found a match and Patrick was transplanted, but the fact of the matter is that the procedure was still both new and rare at that point. That means that there really was no reliable data set for us going into this. Patrick and other transplant around the same time as him are still pioneering — writing the book for others, if you will.
The good news is that the story Patrick is writing is a good one. At his checkup, the GI was on his case ten years ago and knew him well. It’s been at least five years since he’s seen Patrick and he got a bit emotional talking about how much he’s grown and how well he’s doing.


I marvel at the fact that Patrick vaguely recognizes but doesn’t remember having TPN. His memories of hospitalizations, surgeries, and transplant are only distant memories. He has only hints of memories of living in Nebraska or the Ronald McDonald House. Those things are all familiar and sometimes he’ll even be triggered by something, but he doesn’t know why.
For Brian and myself, however, those memories are still very poignant.
In September, we when we were in the hospital for his checkup, Patrick hadn’t eaten much lunch and was hungry, so we stopped into the cafeteria to get him a slice of pizza before the appointment. There are so many memories still in that place. I could see the table I sat at the call Patrick’s wish granter to tell her we needed to cancel his star-raising party because he’d received his transplant. Across the room was the table where we ate Thanksgiving dinner with Brian’s brother’s family, who drove in from Colorado to cook for us.

Just past the cafeteria, there was the door that used to lead to the dingy outdated section of family hotel rooms in the Leed Tower (I don’t think that even exists anymore), where we rented a room for the first week until they had space for us in the Ronald McDonald House. I remember the sagging mattress and the 70’s era carpet and the chip in the sink faucet and the fridge we stocked with sandwich fixings so we could pack a lunch to eat in the ICU break room.
It seems like just yesterday.
On our way out of the building, we showed Patrick the lobby where he met Santa Claus with Toys for Tots at Christmas and therapy pets every Wednesday and — most memorably of all — where he went trick or treating the morning before transplant in a too-small borrowed Buzz Lightyear costume.
What a contrast between that year and this one. Don’t get me wrong. Both years, he was spoiled beyond belief. He may have received almost as many toys, pencils, bubbles, and more from the staff at UNMC in the lobby in 15 minutes as he could get an entire night trick or treating.
Ten years later, Patrick was trick or treating at Disneyland. How amazing is that? He has sacks and sacks of treats and has been eating them since he got home. And that’s OK!!

We celebrated Patrick’s first transplant anniversary at Disneyland, too. I remember it being such a big deal that we laid only about ten pieces of candy and he chose one to eat because he couldn’t handle the sugar.

This week, Patrick made Brian run him from one roller coaster to another all week. (And because he’s spoiled, his dad does just that.) I couldn’t help thinking of that visit where we asked if it was safe for Patrick to ride the upside down rollercoaster. How big of a decision that was. How scare I was. And now he rides it over and over again, and it’s us whose bodies can’t take more.
We splurged a bit and treated him to Goofy’s Kitchen this trip. He ate macaroni and cheese and chicken tenders until he was too full for dessert. I should maybe have warned him they were bringing a cupcake, but I didn’t want to ruin the surprise. It was worth it anyway because Minnie Mouse came when they sang to him. She’s his favorite.

When he isn’t chasing roller coasters at the park, Patrick’s’s chasing characters. He loves to see names written and so he loves collecting autographs. I can’t help but contrast the way he made sure every nurse, CNA and doctor who entered his room wrote their name on the whiteboard when he was little. He’s always loved names. I think I prefer chasing autographs in the park, though.
Patrick doesn’t remember his wish trip. He doesn’t remember wishing. One of our regrets in his making that wish was that he was too young to understand it. We were so sure that if he didn’t wish, the opportunity would pass.
So ten years later, we offered him a chance to wish. Actually, first we offered to take him back to Disneyworld and show him where he’d gone for his wish trip. But Patrick didn’t want to relive a wish he didn’t make. He wanted to wish for himself, and his wish was Disneyland.







It’s been ten years and he’s looking forward — Living forward.
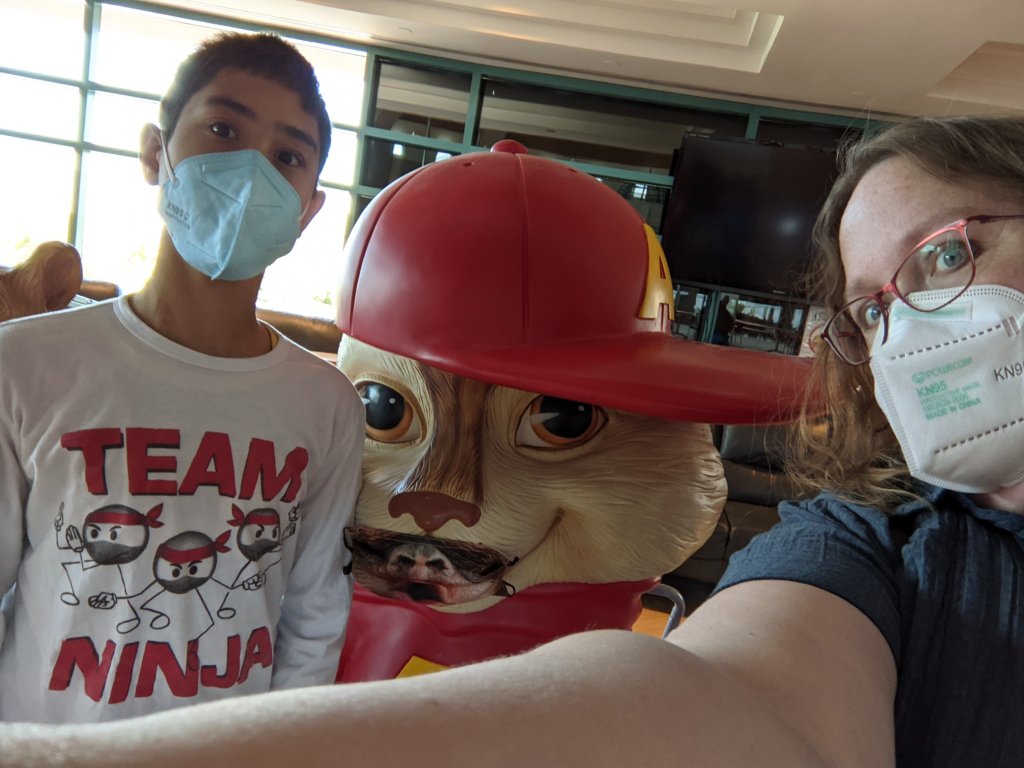
We have had some good moments this year for looking back. Through the support groups I work with, Patrick’s been starting to connect with other patients with short gut and intestinal transplants this year. He’s nervous about it, but I can tell it’s helpful for him to be a part of that community, too.
I also had a very tender moment at the Oley Conference this summer where I talked with an adult transplant patient. She told me about her relationship with her donor’s family and I had a chance to express to her my deep gratitude for Patrick’s.
There really are no words for that. My heart is all tangled up in the depth of their loss and the magnitude devastation turned to beauty. Every additional year, I marvel more at that gift of life. Patrick’s life and ours are forever changed and we are forever grateful.
What an amazing ten years it has been!
From hospital regular to completely lost in hospital halls. From a backpack full of TPN to pockets full of art supplies. From unable to eat to snacks scattered all around the house. From time is running out to we can’t wait to see what the future holds.
And also – when did I become mom to a sixteen year old?